I’ve long-delayed writing this article because it’s a complex subject that could easily overwhelm the reader. However, the more we acknowledge the hormone disease associated with SARD, the better it is for these dogs and their owners. If you need an introduction to this topic, please start with my previous article about terminology.
The Hormone Problem
The underlying endocrine problem in SARD dogs has many similarities to a disease in humans called Congenital Adrenal Hyperplasia or CAH. Congenital means the problem is present at birth (more on this in a minute). Adrenal obviously describes the adrenal glands. And hyperplasia means enlargement of the adrenal glands.
Why do they become enlarged? They become enlarged because they cannot produce sufficient cortisol hormone. These patients are missing an enzyme — a natural chemical — that creates cortisol hormone. Cortisol is energy. It keeps us alive. So, the brain repeatedly instructs the adrenal glands to try. The more they try the larger they become, much like a body builder at the gym. (With time the adrenal glands may wither but that’s another discussion.)
So, in both human CAH patients and in SARD dogs, cortisol production is reduced. If you think that’s not the case for your dog, click on this article and read the Cortisol section very carefully.
Now I said CAH is a disease but it’s really a family of problems. CAH is subdivided by onset (the age at which it starts). It’s also subdivided by enzyme (which enzyme fails). And it’s also classified by severity. Understanding these distinctions is important.
Onset — At What Age Does It Start
As I mentioned, the first documented cases of CAH were diagnosed at birth. For these infants, adrenal enzymes fail while still in their mother’s womb. And for them onset truly is congenital. The problems are visible at birth. I don’t believe this particular version has ever been diagnosed in dogs.
As time passed medical doctors began recognizing CAH in older children and young adults. Since the disease already had a name, doctors began calling the original visible-at-birth version “classic” CAH. And they called these late-onset cases “non-classic” CAH. SARD dogs definitely present as late-onset or Non-classic CAH.
Interruptions in the Cortisol Pathway
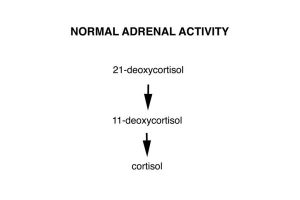
Normally, cortisol is created when the adrenal glands convert a hormone called 21-deoxycortisol (dee-ox-ee-kort-ah-zol) into a hormone called 11-deoxycortisol. And then that is converted into cortisol. (See figure 1). That’s an abbreviated description but it will suffice.
Figure 1.
Medical doctors realized that CAH patients experience interruptions in cortisol production. In humans, the most common point of interruption occurs when the hormone 21-deoxycortisol should be converted to 11-deoxycortisol (figure 2). Normally, an enzyme called 21-hydroxylase (hi-drox-ah-lace) does this job. But when it fails, 11-deoxycortisol is not created and in turn, cortisol is not created.
Figure 2.
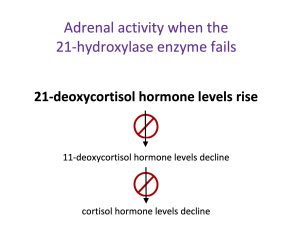
And while this is the most common version in people, this is probably not what we see in dogs. Why? Because hypertension (high blood pressure) is not a common finding in this scenario, but it is a common finding in SARD dogs. (This is a topic for another post.) Therefore, comparing SARD to 21-hydroxylase failure is probably not accurate.
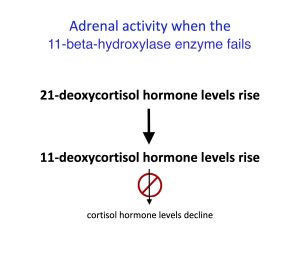
In about 5% of humans, the interruption occurs further down the production line — the point when 11-deoxycortisol should be converted to cortisol (figure 3). Normally, an enzyme called 11-beta-hydroxylase does this. But if this enzyme is deficient, cortisol levels decline. I suspect this is what we see in SARD dogs: 11-beta-hydroxylase deficiency.
Figure 3.
With nowhere to go, the rising levels of precursor hormones — the building blocks — are sent down other pathways of the adrenal gland. This raises levels of other adrenal hormones called sex steroids. Virtually all SARD dogs test positive for elevated adrenal sex steroids. (1-4) These steroids mimic Cushing’s disease.
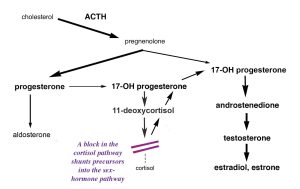
Humans with CAH experience a rise in adrenal testosterone. Dogs take it one step further and convert much of that testosterone into adrenal estrogen. This is one reason we see SARD in dogs but not in humans. Read more here.
Estrogen is a known excitotoxin. It causes seizure activity. Thirty years ago, researchers first described retinal seizure activity (excitotoxicity) as a cause of SARD. (5,6)
Severity of the Interruption
Finally, medical doctors realized that CAH’s block in cortisol production could vary in severity. The block could be profound, sometimes resulting in death or it could be so mild as to cause only lethargy. Doctors suspect that mild, late-onset CAH is the most common form of CAH in humans.
For SARD dogs, the severity of the block may also vary. A profound block can cause many system-wide health problems for dogs, including organ failure or sudden death. Or the block can be mild, permitting a dog to tolerate slightly elevated sex steroids for years.
Treating the Underlying Disease
Low-dose, daily cortisol replacement has been the standard of medical care for CAH patients for over 50 years. Daily cortisol replacement offers CAH patients a relatively normal life. The same is true for dogs. Low-dose, daily cortisol replacement reduces excess sex steroids and their symptoms in 95% of SARD dogs and returns vision in 22% – 55% of cases.
On the other hand, immuno-suppressant treatments do not address the hormone problem associated with SARD. And Cushing’s drugs? They can be dangerous to these dogs because they interfere with what little cortisol these dogs do make.
So, in review:
• Both dogs and humans experience interruptions in cortisol production.
• In humans it’s usually due to the 21-hydroxylase enzyme, in dogs, it’s likely the 11-beta-hydroxylase enzyme.
• Both dogs and humans experience rising levels of sex steroids.
• In humans, adrenal testosterone rises. In dogs, adrenal estrogen also rises.
• Elevated estrogen causes excitotoxicity or cell death from seizures.
• Excitotoxicity is one cause of retinal degeneration.
• Low-dose cortisol replacement reduces elevated sex steroids in 95% of dogs and returns vision in 22% – 55% of cases.
I hope this helps you.
Best,
Caroline
|
Characteristics of Congenital Adrenal Hyperplasia (Low cortisol production) |
Humans |
SARD Dogs |
|
Most common onset |
Late-onset |
Late-onset |
|
Most common enzyme failure |
21-hydroxylase |
11-beta-hydroxylase, likely |
|
Most common severity |
Mild |
Varies |
|
Adrenal sex steroid production |
Ends in testosterone |
Continues on to estrogen |
1. Carter RT, Bentley E, Oliver JW, Miller PE, Herring IP. Elevations in Adrenal Sex Hormones in Canine Sudden Acquired Retinal Degeneration Syndrome (SARDS). Proceedings of the 34th Annual Meeting of the American College of Veterinary Ophthalmologists 2003;34: 40. (Scroll down to abstract #51 if you use the link.)
2. Oliver JW, Steroid Profiles in the Diagnosis of Canine Adrenal Disorders. Proceedings of the 25th Annual Meeting of the American College of Veterinary Internal Medicine 2007; 471-473.
3. Carter RT, Oliver JW, Stepien RL, Bentley E. Elevations in Sex Hormones in Canine Sudden Acquired Retinal Degeneration Syndrome (SARDS). Journal of the American Animal Hospital Association 2009; 45: 207-214.
4. Kamaromy AM, Abrams KL, Heckenlively JR, Lundy SK, Maggs DJ, Leeth CM, MohanKumar PS, Peterson-Jones SM, Serreze DV, van der Woerdt A. Sudden Acquired Retinal Degeneration Syndrome (SARDS) — a Review and Proposed Strategies Toward a Better Understanding of Pathogenesis, Early Diagnosis, and Therapy. Veterinary Ophthalmology 2015; 19: 319-331.
5.Riis RC. EM observations of a SARD case (abstract). 21st Annual Meeting of the American College of Veterinary Ophthalmologists 1990; 21: 112–113.
6. Abrams KL, Dreyer EB. Excitotoxicity in canine sudden acquired retinal degeneration. Investigative Ophthalmology and Visual Science 1993; 34(Suppl): 3297.





